Value-Based Payments: How Your Agency Can Benefit
Post - Value-Based Payments: How Your Agency Can Benefit
Value-based payments (VBPs) are a type of reimbursement model insurance companies use. Under this model, providers are paid based on the quality of care they deliver rather than the quantity of services they provide. To receive reimbursement, providers must meet specific quality benchmarks, such as reducing hospital readmissions or providing cost-effective care.
VBPs are typically tied to specific health outcomes, such as reducing the incidence of a particular disease. For example, an insurance company might offer a higher reimbursement rate to providers who successfully lower their patients’ blood pressure. This incentive encourages providers to focus on preventive care and disease management rather than treating the illness after it occurs.
Ultimately, VBPs have the potential to improve patient outcomes and lower healthcare costs.
Related Article: Preparing Your Home Care Agency for Reimbursement Rates Based on Quality Scores
How Can Agencies Use Value-Based Payments to Improve Training Experiences for Caregivers?
One way agencies can use VBPs to improve training experiences for caregivers is by providing incentives for quality care.
For example, agencies could offer bonuses for caregivers who identify preventive care opportunities or successfully lower critical indicators in their patients, such as high blood pressure. This would encourage caregivers to focus on providing quality care, rather than simply meeting minimum standards.
In addition, agencies could use VBPs to fund continuing education opportunities for caregivers.
For example, agencies could offer bonuses for caregivers who complete a certain number of training hours each year. This would encourage caregivers to keep up with the latest changes in their field and improve their skills.
How Can Agencies Use Value-Based Payments to Improve Onboarding and Orientation Experiences?
Under a VBP system, providers are paid based on how well they meet certain quality metrics. These metrics can include patient satisfaction, length of stay, and readmission rates. VBPs can improve the onboarding and orientation experiences for new caregivers.
By tying provider payments to quality measures, agencies can incentivize providers to deliver a better onboarding experience. This can help to ensure that new caregivers are fully oriented to their job duties and have a positive first impression of the agency.
In addition, VBPs can help to improve provider retention rates. By rewarding providers for high-quality care, agencies can create a more positive work environment that attracts and retains top talent.
How Else Can Agencies Benefit From Implementing Value-Based Payments Into Their Business Model?
In recent years, there has been a shift away from traditional fee-for-service models of reimbursement in the healthcare industry. Instead, many payers are now moving towards VBPs, which tie reimbursement to quality and outcomes measures. While this shift may require some initial investment and adjustment, there are many potential benefits for agencies that implement VBPs into their business model.
One benefit is that it can help to align the incentives of all involved parties. Under fee-for-service models, providers may be tempted to order unnecessary tests or procedures to increase their reimbursement. In contrast, under a value-based model, providers are financially incentivized to focus on quality care that leads to positive outcomes for patients. This can help improve the overall quality of care while reducing costs.
Another benefit is that it can help to attract and retain high-quality providers. In today’s competitive home care marketplace, many providers are looking for agencies that offer VBPs. By providing this type of compensation, agencies can attract and retain high-quality providers committed to delivering quality care.
VBPs can also help agencies to improve other aspects of their operations. For example, by basing payments on quality measures, agencies can encourage providers to collect and use data to continuously improve their care delivery. Additionally, VBPs may help to increase transparency and communication between providers and payers.
How showd.me Can Help Agencies Transition to Value-Based Payments
showd.me provides custom training solutions for home care agencies who want to:
- Make onboarding simple and effective
- Retain more staff
- Meet their compliance obligations without increasing their administrative burden
- Educate staff with the latest evidence-based best practices
- Rein in their training costs while still delivering high-quality training
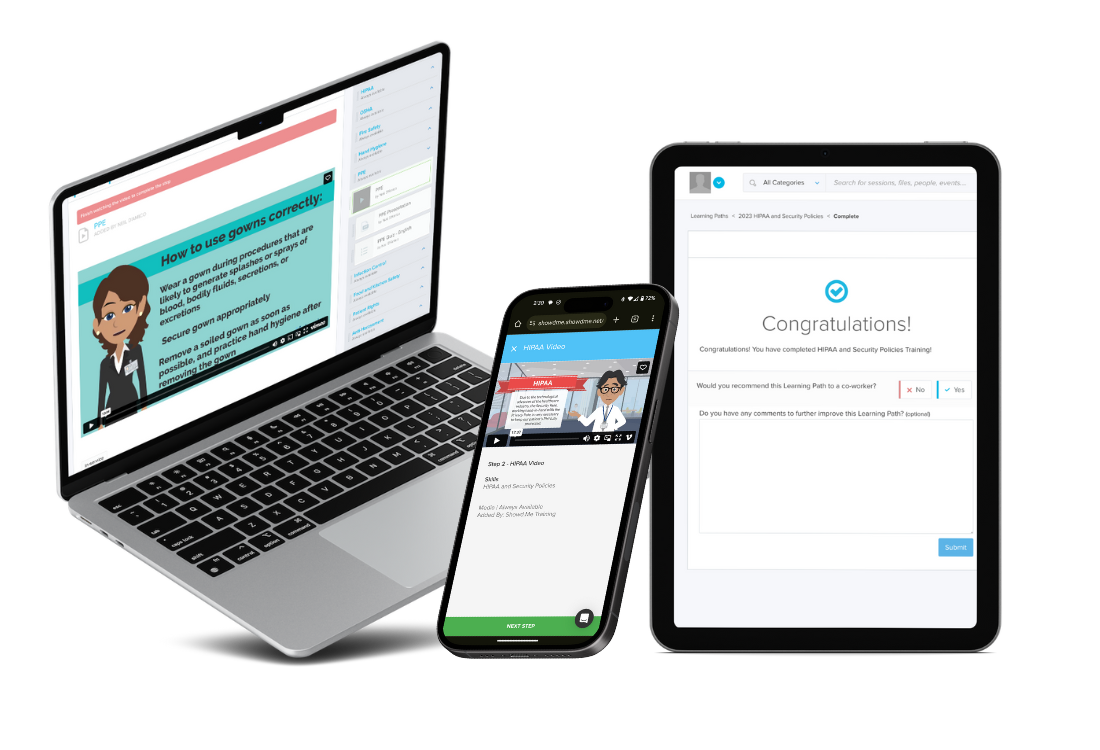
showd.me offers many features that can help agencies to transition to a value-based model, including:
- Customizable course content that can be tailored to meet the specific needs of an agency
- A learning management system that helps agencies to deliver and track caregiver training
- On-demand training so that caregivers can learn on any device anytime
- Real-time data on caregiver engagement and performance that helps managers identify staff who need additional support
- Cost-effective subscription plans that scale as an agency grows
With its easy-to-use platform and customizable course content, showd.me is the perfect solution for agencies who want to improve their quality of care while also reducing costs.
Request a demo today.
Let Us Show You More
See how showd.me's unique service-first approach helps hundreds of healthcare organizations ensure compliance. Request a demo today!

